What are the differences between euploid, aneuploid and mosaic embryos?
 Infertility patients and their doctors are always looking for ways to achieve successful in vitro fertilization (IVF) cycles. Many physicians recommend preimplantation genetic screening (PGS) to test a patient’s embryos, especially if the embryology laboratory has created multiple ones. PGS is one of the most effective ways to find the best embryos for transfer.
Infertility patients and their doctors are always looking for ways to achieve successful in vitro fertilization (IVF) cycles. Many physicians recommend preimplantation genetic screening (PGS) to test a patient’s embryos, especially if the embryology laboratory has created multiple ones. PGS is one of the most effective ways to find the best embryos for transfer.
PGS, using high-resolution next-generation sequencing, analyzes which embryos are healthy and which are not by examining the outer layer of their cells.
Euploid embryos
Embryologists are looking for euploid embryos; chromosomally normal with 46 chromosomes in 23 pairs. Their goal is to transfer one euploid embryo that will have the best chance of becoming a healthy baby.
Aneuploid embryos
Aneuploid embryos that don’t have the correct number of chromosomes can lead to increased rates of miscarriages, birth defects and IVF failure. One or more chromosomes can be duplicated or missing. Trisomy is defined by the presence of the extra chromosome. Monosomy means missing a chromosome. Down Syndrome (Trisomy 21) and Turner Syndrome, where an x chromosome is missing, are examples of aneuploid embryos or aneuploidy.
In nature, most aneuploid embryos are lost, and a woman has a negative pregnancy test. Those that survive result in miscarriage and the few who grow might result in a baby born with Down Syndrome or a similar problem.
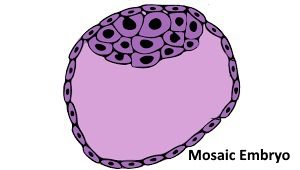
Mosaic embryos: a unique category of embryos
PGS also can detect embryos that are considered mosaic. Mosaic embryos, which comprise about 20% of embryos, have both normal and abnormal cells. Older women who use their eggs might have a higher percentage of them.
Mosaic embryos fall into a unique category. They are not abnormal because they have the potential to grow into babies. But there is a big question of whether the babies will develop normally or not.
A few fertility doctors around the country have given patients the option of using their mosaic embryos if the patients had no other embryos or it was unlikely they could create more. As a result, a small number of healthy babies have been born. It is still too early to determine if using mosaic embryos, even when there are no alternatives for the patient, is a safe choice, so the majority of fertility clinics are not using them.
Researchers who see potential in mosaic embryos question whether PGS, which only looks at five to 10 cells from the outer shell of a 200-cell embryo, is an accurate reflection of the inner cell mass. They contend that even if there are mistakes in cell division early in the embryo’s development, it may have the ability to self-correct and produce a healthy baby. More research needs to be conducted to determine how the inner cell mass of the embryo evolves.
Patients should discuss the status of their embryos with their physician before their embryo transfer. Reproductive medicine is a rapidly advancing field, and HRC Fertility is committed to using the latest evidence-based research in its practice, but only when it has been proven safe and effective for both the prospective parents and their future children.
References
https://www.medicaldaily.com/what-are-mosaic-embryos-and-why-are-they-dividing-ivf-experts-426602
https://people.com/health/what-to-know-mosaic-embryos/
